|
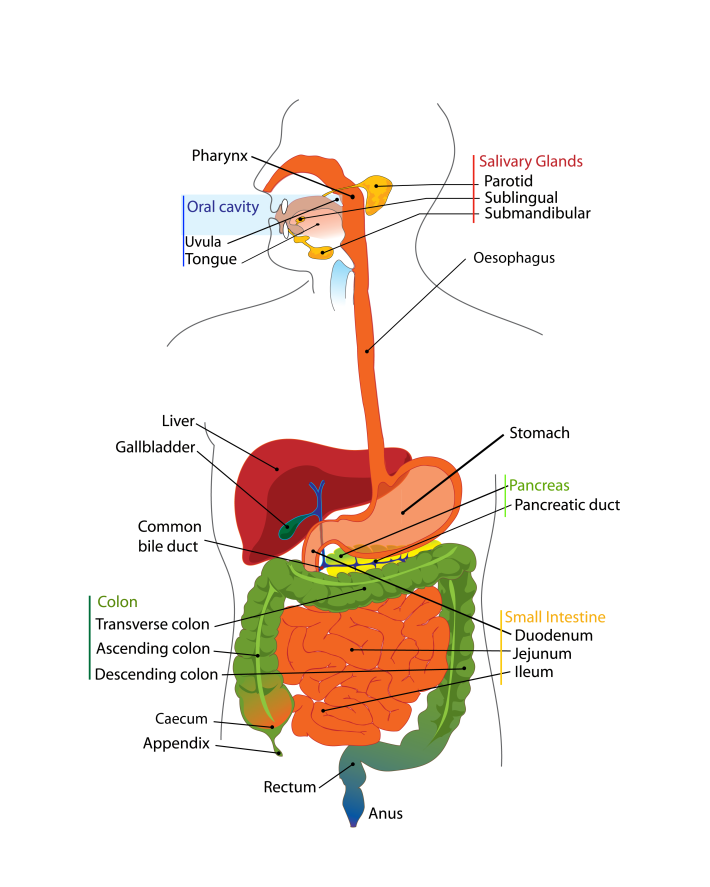
Do you think about what happens to food after you have eaten it? Probably not, but to understand how microbes contributing to the gut microbiota survive inside you, it is important to have a basic understanding of how the human digestive tract works. The following won’t go into details as to how the organs of your digestive tract work together to convert food to energy and nutrients to keep your body fuelled and healthy. Instead, it will concentrate on how the nutrients in your food are made available to the microbes that inhabit every inch of your digestive tract. The easiest way to think about your digestive tract is to picture it as a tube that runs through your body, from your mouth to your anus (Figure 1). If it were not for the valves and sphincters that are found throughout your digestive tract, your body would essentially be a hollow tube. Valves ensure the food you eat goes in only one direction of travel, while sphincters are rings of muscle that surround and protect the opening or closing parts of your digestive tract, such as your stomach or anus. Your whole digestive tract is about 9 metres long. What we refer to as the gastrointestinal tract includes the regions of the digestive tract between the oesophagus and the anus. Activities of and/or secretions from the liver, gallbladder and pancreas aid the digestive process, and these organs are considered part of the digestive tract. There is a strong association between the activities of gut microbes and the healthy functioning of the liver and other organs of the body. Saliva You take food into your mouth and chew it to produce a bolus (a ball of chewed food). The majority of the food you eat comprises carbohydrates, fats, protein and water, with varying small amounts of vitamins, minerals, nitrates, nucleotides, methylamines and additives. The action of chewing causes saliva to be secreted from your salivary glands into your mouth. Saliva has a number of functions that aid in the digestion of food and in protecting you from harmful bacteria (Valdez & Fox, 1991; Abiko & Saitoh, 2007). It lubricates the bolus so that it passes down your oesophagus easily, with this smooth passage also protecting the lining of your mouth and oesophagus from wear and tear. The enzymes salivary amylase and lingual lipase start to break down starch and fats in the bolus to simpler sugars and less-complex fats, respectively (Valdez & Fox, 1991; Phan & Tso, 2001). These simple fats and sugars (and undigestible carbohydrates) pass into your stomach, along with proteins. After you swallow the bolus, peristalsis (a wave-like motion caused by the rhythmic contraction and relaxation of the smooth muscles that run along your oesophagus) propels the bolus down your oesophagus to your stomach. The stomach Your stomach is essentially a short-term storage reservoir for food and contains gastric acid, with a pH between 1 and 4 due to hydrochloric acid secreted by parietal cells lining the stomach (Encyclopaedia Britannica). In addition to hydrochloric acid, gastric acid comprises sodium chloride and potassium chloride. The acidity of the stomach serves three main roles: i) aiding in the digestion of food particles, ii) protecting you from potentially dangerous foreign microbes (by foreign microbes I mean organisms that are either not normal members of the gut microbiota or normally present at very low levels), and iii) aiding in the digestion of proteins. Acidity of the stomach environment activates pepsinogen to the digestive enzyme pepsin. It also aids in unravelling (denaturing) proteins so that they are more easily broken down to their constituent amino acids by enzymes such as pepsin. Gastric lipase aids in the digestion of dietary lipids. Vigorous contractions of gastric smooth muscle mix and grind foodstuffs with gastric secretions, resulting in the formation of chyme, a thick, semi-liquid mass of partially digested food. The small intestine The small intestine (comprising the duodenum, jejunum and ileum) is a long, winding tube that is ~3 metres long and 2–3 cm in diameter (Espey, 2013). It is the longest organ in your body. Food, in the form of chyme, passes from the stomach through the pyloric sphincter to the duodenum. The acidity of the chyme is reduced by bile acids secreted from the gallbladder, and enzymes secreted from the pancreas and duodenal cells help digest components of the chyme. For example, pancreatic amylase continues the break down of digestible carbohydrates to simple sugars, while trypsin and chymotrypsin (secreted from the pancreas in the inactive forms trypsinogen and chymotrypsinogen, respectively) break down proteins to their constituent amino acids. Peristalsis pushes chyme along the small intestine. The surface area of the small intestine is large compared with its length due to its villi and ‘brush border’, which comprises thousands of finger-like projections called microvilli (Figure 2). Consequently, the small intestine is the primary site within the human gastrointestinal tract for nutrient (e.g. glucose, amino acids, fatty acids), water and electrolyte (sodium, chloride, potassium) uptake into the blood. Up to 95 % of absorption of nutrients occurs in the small intestine. 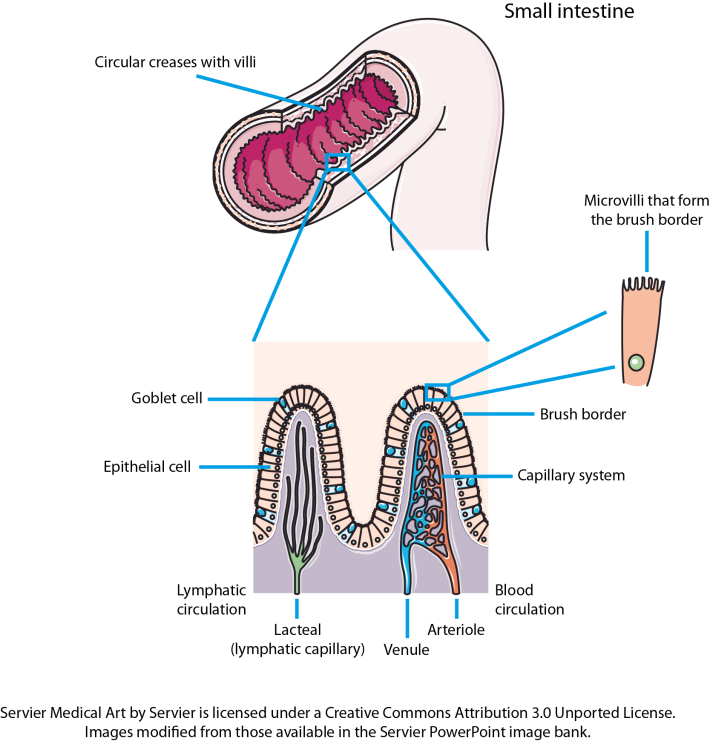 Figure 2. The small intestine is convoluted, with the folds forming thousands of villi that project into the intestinal lumen. There are 20–30 villi per square millimetre of small-intestinal tissue (Espey, 2013). Each of the epithelial cells covering the villi is covered with microvilli that form the brush border of the small intestine. The huge surface area created by the villi and the microvilli increases the amount of nutrients that can be taken up by the small intestine. Goblet cells secrete mucus into the intestinal lumen, lubricating the small intestine. Other cells present, but not shown on the image, include enteroendocrine and stem cells. The caecum, appendix and large intestine (colon)The caecum is a pouch that connects the ileum to the proximal colon, and is the beginning of the large intestine. It receives undigested dietary material from the ileum, via the ileocaecal valve. The caecum is connected to the appendix and is separated from the contents of the ascending colon by the caecocolic junction. In herbivores, undigested dietary material that reaches the caecum is fermented by the caecal microbiota. The human caecal microbiota is capable of fermenting dietary carbohydrates (Flourie et al., 1986), but the contribution this makes to gut fermentation of dietary substances that escape digestion in the upper gastrointestinal tract is minimal when you consider the contribution of the colonic microbiota to this process. Consequently, the human caecum is considered a dead-end pouch that connects the upper and lower intestinal tract. However, it is likely that the caecal microbiota is important in establishing/maintaining the appendix and colonic microbiota, and may play a role in human health. The appendix is a 5–10 cm long, 0.1–0.5 cm wide pouch that is an extension of the caecum (Randal Bollinger et al., 2007). It does not play a role in digestion. Instead, it is part of the immune system, and acts as a ‘safe house’ for the commensal microbiota that can re-inoculate the colonic microbiota after a bout of diarrhoea (Laurin et al., 2011). In humans, the large intestine serves as the main site of microbial fermentation of dietary substrates that escape digestion in the upper gastrointestinal tract. The large intestine is also involved in the uptake of water from digesta and waste material prior to the expulsion of faeces from the body (defecation). References Abiko, Y. & Saitoh, M. (2007). Salivary defensins and their importance in oral health and disease. Curr Pharm Des 13, 3065–3072. Encyclopaedia Britannica: Human Digestive System – proteins. Espey, M. G. (2013). Role of oxygen gradients in shaping redox relationships between the human intestine and its microbiota. Free Radic Biol Med 55, 130–40. Flourie, B., Florent, C,, Jouany, J. P., Thivend, P., Etanchaud, F. & Rambaud, J. C. (1986). Colonic metabolism of wheat starch in healthy humans. Effects on fecal outputs and clinical symptoms. Gastroenterology 90, 111–119. Laurin, M., Everett, M. L. & Parker, W. (2011). The cecal appendix: one more immune component with a function disturbed by post-industrial culture. Anat Rec (Hoboken) 294, 567–579. Phan, C. T. & Tso, P. (2001).Intestinal lipid absorption and transport. Front Biosci 6, D299–D319. Randal Bollinger, R., Barbas, A. S., Bush, E. L., Lin, S. S. & Parker, W. (2007). Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol 249, 826–831. Valdez & Fox (1991).Interactions of the salivary and gastrointestinal systems I. The role of saliva in digestion. Dig Dis 9, 125–132. This older website, run by Colorado State University, is very good for more-detailed information on the human digestive system. Comments are closed.
|
Lesley HoylesProfessor of Microbiome and Systems Biology, Nottingham Trent University ArchivesCategories
All
|